All about atopic dermatitis: causes, symptoms and treatments
Atopic dermatitis, also known as atopic eczema is a chronic inflammatory skin condition. But what is atopic eczema? What are the symptoms? What are the causes? How can you tell it apart from other types of eczema? What can be done to alleviate it and space out the flare-ups?
- 4
of the population in Europe is affected
- 10 to 15%
of children suffer from atopic dermatitis
- 80
is the risk of a child being affected if both parents have atopic dermatitis
What is atopic eczema?
What are the symptoms?
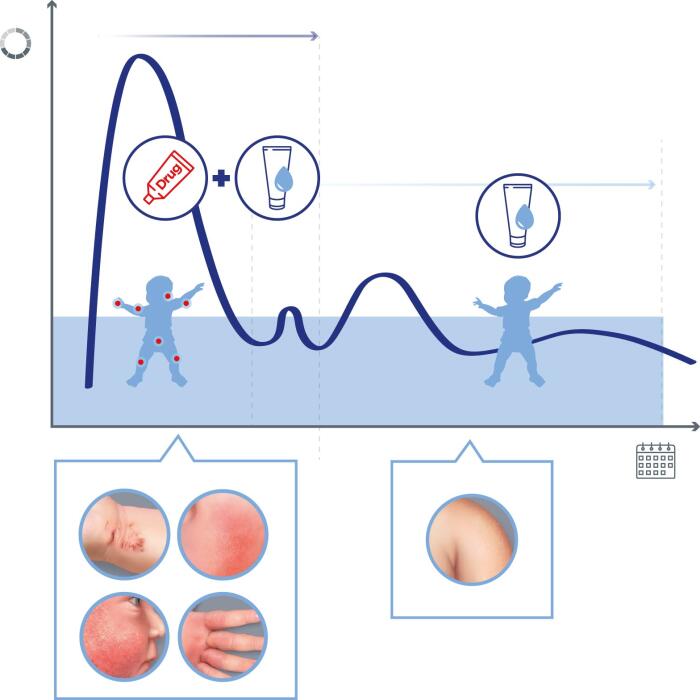
Atopic eczema is a chronic inflammatory skin condition (hence its other name, dermatitis), which develops in flare-ups, i.e. alternating between remission and symptomatic phases2. These phases vary in duration.
Atopy occurs when there is a hereditary predisposition to develop symptoms of immediate hypersensitivity, such as hay fever, asthma, etc.3
Studies have shown that 50-70% of people with atopic dermatitis have a first-degree relative (father, mother, brother or sister) who also suffers from it1. Furthermore, if both parents are affected, the risk of the child developing atopic eczema increases to 80%4.
Atopic eczema affects mostly children. It most often appears from the age of 3 months onwards, and is therefore known as infant eczema. It develops in flare-ups during childhood and usually disappears in adolescence. However, it may persist into adulthood.
- Skin lesions
- Itching
- Dry skin
Atopic eczema has three main characteristics¹:
- Itching (or pruritus), which is accompanied by sleep disturbances in infants and an urge to scratch. In older children and adults, this itching leads to scratching lesions and even grazes.
- Inflammatory skin lesions: redness and thickening of the skin in characteristic areas (see above) giving the skin a rough, red appearance, accompanied by small blisters. The latter, when they break, produce oozing and leave a scab.
- Dry skin (or xerosis) outside the areas affected by eczema.
Scratchin lesions due to atopic eczema can sometimes become infected with bacteria (staphylococcus) or viruses (herpes). It is, therefore, essential that a doctor is consulted if there are changes in the appearance of the eczema patches, especially if they are accompanied by pain, fever and/or a change in general condition1.
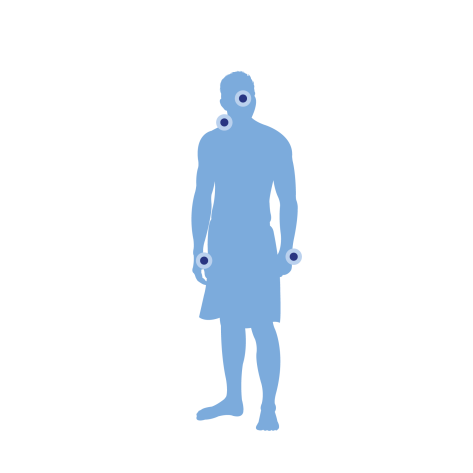
Where do atopic dermatitis patches develop?
The lesions of atopic eczema are found on characteristic areas of the body, which evolve with age5
- In infants: the main areas affected are the face (forehead, cheeks, chin) and the outer surface of the arms and thighs.
- In children: they are mainly found on the elbow and wrist folds and on the back of the knees.
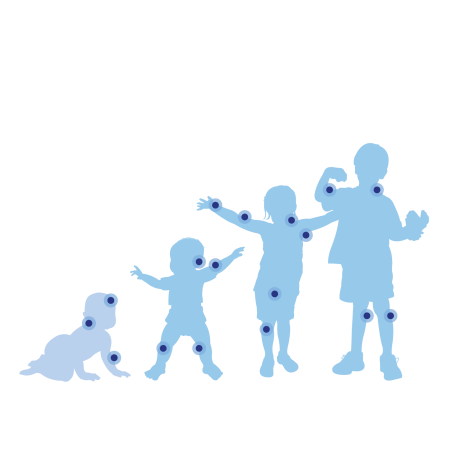
- In adults, if atopic dermatitis persists, it is often the neck and face alone that are affected by eczema. Sometimes the affected area can be generalised but more pronounced on the elbow and knee creases. The hands are also frequently affected and the symptoms can be aggravated by work.
The different types of eczema
- Contact eczema
- Varicose eczema
- Nummular eczema
What are the other types of eczema?
Atopic eczema is not the only form of eczema, although it is the most common. It is, therefore, important to know the difference.
- Contact eczema results from repeated contact with an allergenic substance (allergen). Its symptoms are similar to those of atopic dermatitis but its location is limited to the contact area. Construction and health professionals are particularly affected because they are in regular contact with rubber gloves, metals, chemicals, antibacterial products, etc. The best way to resolve contact eczema is to avoid all contact with the substance(s) involved6.
- Varicose eczema, which is mainly located on the legs, is due to venous insufficiency.
- Nummular eczema: these are rashes in the form of rounded red patches, resembling coins.
What causes atopic eczema?
Atopic eczema is the consequence of a range of immunological and skin dysfunctions.
A person suffering from atopic eczema has an altered skin barrier characterised by a reduction of the natural protective hydrolipidic film. The skin can therefore no longer fulfil its barrier function, which makes it more sensitive to external aggressors. Environmental molecules called allergens such as pollen, dust, etc. can, therefore, penetrate the skin more easily and come into contact with the skin's immune cells. This triggers an inflammatory, maladaptive response that causes the symptoms of eczema. This lack of hydrolipidic film is also accompanied by significant skin dryness1.
In addition to having skin that is more permeable to allergens, people with atopic dermatitis also secrete high amounts of antibodies called IgE or immunoglobulin type E. This is a specific immune system response to the presence of allergens. This high level of IgE causes the body to overreact to the allergen aggressor1,3.
Over the past 30 years, there has been a significant increase in the number of cases of atopic dermatitis in developed countries.
Changes in infant feeding, particularly the decline in breastfeeding during the first three months of life and earlier dietary diversification, may partly explain this phenomenon4.
Another hypothesis put forward by scientists to try to explain this increase is that the more hygienic environment of infants and young children may reduce and delay the exposure of their immune system to a wide variety of substances, making it more sensitive4. This so-called hygiene hypothesis could also be the cause of other allergic manifestations.
How do you treat atopic eczema?
Local treatment of atopic eczema is symptomatic, i.e. it relieves symptoms such as itching and patches without making the condition disappear permanently. It also helps to limit the occurrence of new flare-ups and, therefore, also to space out the flare-ups7.
The treatment is prescribed by a doctor (usually a general practitioner, paediatrician or dermatologist) after a clinical examination and diagnosis of atopic dermatitis. It is essentially based on the application of corticosteroids (cortisone cream or ointment) to the lesions until they disappear. This takes an average of one to three weeks. The strength of the corticosteroid and its dosage should be determined by the doctor.
If the corticosteroid fails, a local immunomodulator can be prescribed, i.e. a drug that will decrease the immune response on the skin, where the drug is applied.
UVA and UVB phototherapy can also be used by a dermatologist. This involves repeated skin exposure to lamps emitting UVA or UVB radiation. In the case of UVA, exposure is preceded by psoralen (often taken orally). It is a photosensitising compound that is supposed to make the skin more sensitive to UV radiation. It is effective in the short term but must be used in moderation.
Finally, when local treatments are not sufficient, systemic treatments (oral or injectable) can be considered. These include immunosuppressants and biotherapy drugs that act on the patient's immune system to reduce atopic symptoms8,9.
Finally, investigating the responsible allergens may be considered, especially if a correctly performed local treatment has failed.
In addition to the medical management of atopic eczema, it is important to adopt a specific routine to take care of your skin every day.
Atopic eczema requires long-term management: simple measures implemented every day can improve the effectiveness of treatments, space out flare-ups and improve patients' quality of life1.
- Avoid irritating materials (wool, synthetics, coarse fibres) in favour of fine fibre fabrics such as cotton and linen10
- Regularly trim fingernails, especially for children, to minimise scratching injuries
Simple measures can improve the effectiveness of treatments
Regularly cut fingernails
Adapt your hygiene routine1:
- Avoid hot showers or baths as this makes the skin dryer and more itchy. You should continue showering during flare-ups while using suitable products.
- Dry by dabbing, not by rubbing, to avoid irritating the skin.
- It is important to use specific toiletries that are suitable for atopic skin. These are formulated without fragrance, with mild surfactants and have a physiological pH so that they do not irritate the skin but rather hydrate it durably and soothe itching.
Our hygiene recommendations for skin with an atopic tendency
Avoid hot showers or baths as this intensifies itching
Dab to dry
Use appropriate toiletries
Moisturise your skin daily 7:
People with atopic eczema have permanently dry skin all over the body, which impairs the barrier function of the epidermis. The use of emollient, i.e. moisturising, creams helps to restore this function. Emollients should be applied all over the body, once or twice a day. Regular application of emollients helps to space and minimise flare-ups and reduce the use of corticosteroids.
Daily application of an emollient helps to space out flare-ups and reduce the use of corticosteroids. Proper daily moisturising and hygiene will work in synergy.
Some tips to limit atopic eczema flare-ups
Opt for showers
Apply an emollient
Apply the emollient once or twice a day
Our expert
" Like European experts, I recommend the use of emollients as a background treatment to prevent flare-ups of atopic dermatitis "*
Dr Alain DELARUE
Medical Director – Pierre Fabre
*Wollenberg A. et al. European guideline (EuroGuiDerm) on atopic eczema. JEADV. Volume 36, Sep 2022. 1409-1431. e
Playing YouTube videos requires the use of cookies in order to offer you targeted advertising based on your browsing For more information, please visit YouTube's « cookie » policy.
You have rejected Youtube's cookies and therefore you cannot view the video.
You can change your choices by clicking on « Cookie Settings » and accept Youtube's cookies to enable the video.
You can change this setting and withdraw your consent at any time.
EFFECTIVENESS OF DEXERYL EMOLLIENT CREAM in treating ATOPIC DERMATITIS
- -50
flare-ups of atopic dermatitis¹
- -77.5%
skin dryness²
- 2X
fewer patients used corticosteroids¹
- Tiplica G.S. et al. Emollient Use in Children with AD. Pediatric Dermatology 2017
- Tiplica G.S. et al. Prevention of Flares in Children with Atopic Dermatitis with Regular Use of an Emollient Containing Glycerol and Paraffin: A Randomized Controlled Study. JEADV 2018
Are you familiar with the effectiveness of DEXERYL Emollient Cream in treating your condition?
DEXERYL Emollient Cream provides patients with clinical studies that have significantly demonstrated its effectiveness.
DEXERYL Emollient Cream: the skin partner for dry and sensitive skin
The basis for treating xerosis is, above all, moisturising the skin and appropriate hygiene.
DEXERYL supports you with emollient skin care and cleansers specially formulated for sensitive skin and recommended for the treatment of signs of skin dryness (xerosis).

DEXERYL Emollient Cream
DEXERYL Emollient Cream can be used to protect the skin and treat the signs and symptoms of dry skin, particularly in the context of atopic dermatitis, thanks to:
- glycerol for its hydrating action
- vaseline and paraffin for their protective role

Dexeryl supports you each day
Sources:
- https://dermato-info.fr/fr/la-peau-de-l’enfant/la-dermatite-atopique
- https://www.ameli.fr/assure/sante/themes/eczema-atopique/reconnaitre-eczema-atopique
- https://www.larousse.fr/dictionnaires/francais/atopie/6150
- https://www.inserm.fr/dossier/dermatite-atopique-eczema-atopique/
- https://dermato-info.fr/fr/la-peau-de-l’enfant/la-dermatite-atopique
- https://www.associationeczema.fr/les-differentes-formes-deczemas/
- https://www.ameli.fr/assure/sante/themes/eczema-contact/consultation-traitement
- https://dermato-info.fr/fr/les-traitements-en-dermatologie/photothérapie_les-traitements-par-la-lumière
- Fluhr JW, Darlenski R, Surber C. Glycerol and the skin: holistic approach to its origin and functions. Br J Dermatol. 2008 Jul; 159(1): 23-34. doi: 10.1111/j.1365-2133.2008.08643.x. Epub 2008 Jul 1. PMID: 18510666
- https://dermatos.fr/le-dermato-soigne/eczema/
- Discover The Different Types of Eczema: How to Recognise Them?
The Different Types of Eczema: How to Recognise Them?
- Discover Causes of Eczema: Why Does It Occur and How Can You Prevent It?
Causes of Eczema: Why Does It Occur and How Can You Prevent It?
- Discover Eczema Symptoms: Identification and Understanding
Eczema Symptoms: Identification and Understanding