What is eczema?
Discover all about eczema: from its definition and symptoms to identification methods. Accurate and up-to-date medical information.
Eczema definition
Eczema encompasses a group of inflammatory skin diseases characterized by dry, itchy skin, red patches, blisters, weeping, and crusting, typically flaring-up periodically¹ ² ³ ⁴. Various types of eczema exist, and it's possible for someone to have more than one type at the same time¹ ². Commonly, "eczema" refers to atopic eczema or atopic dermatitis, the most common type.
Atopic eczema or atopic dermatitis¹ ² ³ ⁴
Atopic dermatitis is a chronic inflammatory skin disease usually starting in childhood. It stems from skin dysfunction, making it overly sensitive to environmental factors.
While most cases of atopic eczema resolve clear up in childhood (50% by age 5), about 10 to 15% continue into adulthood⁴. Less frequently, the first eczema flare-ups may appear during adult age.
Contact eczema¹
This eczema type arises from contact with irritants or allergens, like chemicals, metals, or fragrances, affecting areas in direct contact with these substances (hands, neck, face).
Other types of eczema² ³
Additional types of eczema include dyshidrotic eczema, nummular eczema, and varicose eczema.
Different types of eczema
Contact eczema
Other types of eczema
Atopic skin vs normal skin: understanding the difference
What is atopy?⁴
"Atopy" indicates a hereditary predisposition to developing various allergic disorders, affecting the skin like atopic eczema or the respiratory system like asthma and allergic rhinitis. Atopy is strongly genetic: 50-70% of individuals with atopy have a first-degree relative (parent, sibling) also affected. The likelihood of developing atopic eczema significantly increases, up to 80%, if both parents are atopic.
Characteristics of atopic skin³ ⁴
Atopic skin differs from normal skin in several aspects :
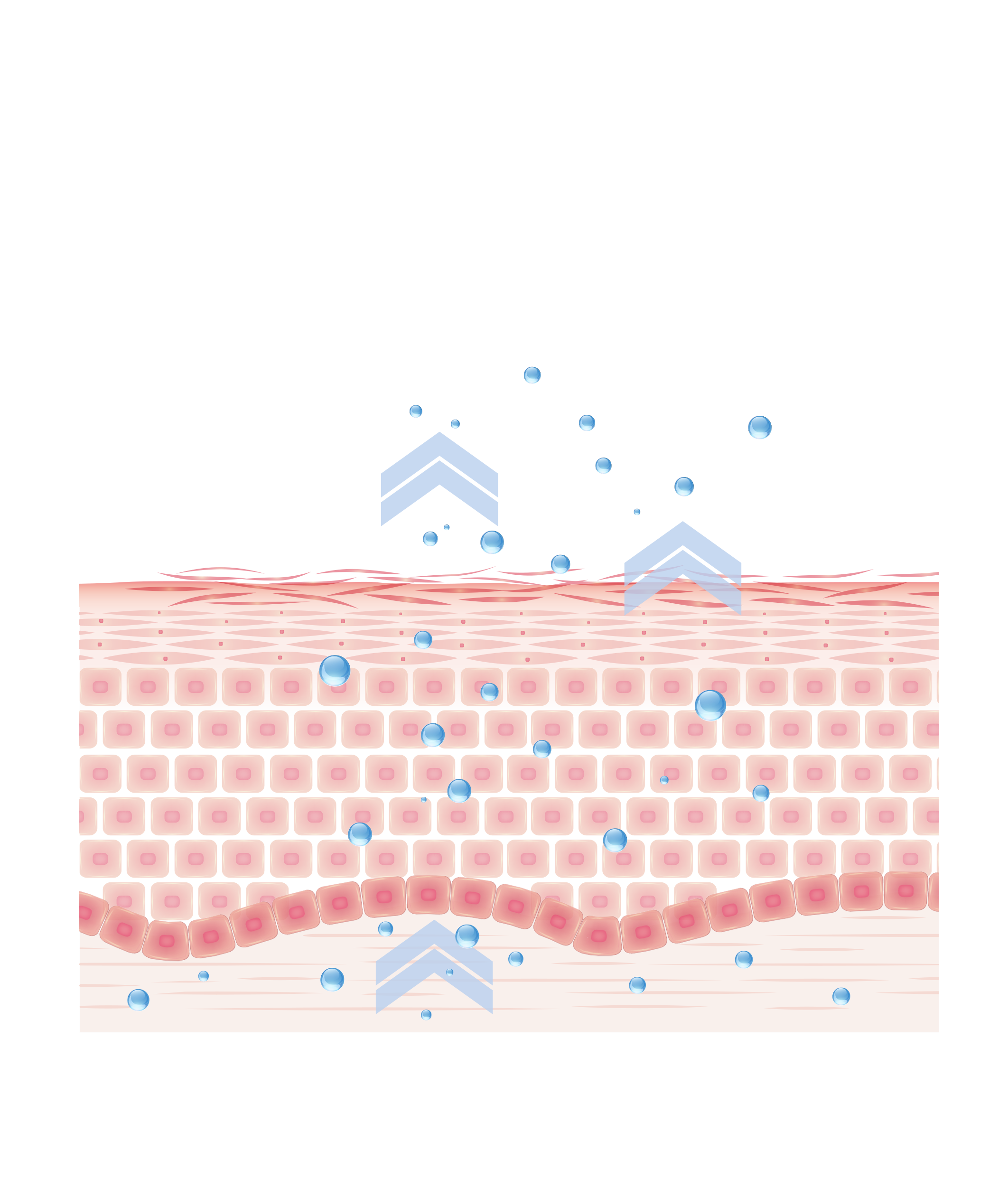
- Dryness : atopic skin poorly retains water, leading to dehydration.
- Increased permeability: atopic skin is more susceptible to allergens (pollens, dust) and external irritants.
- Allergic reactions : the immune system of atopic individuals overreacts to irritants and allergens, triggering eczema
- Sensitivity: atopic skin is more reactive to environmental factors like heat, chemicals, rough textiles, etc…
Identifying atopic eczema: symptoms and key indicators
Symptoms of atopic eczema¹ ³
Atopic eczema cycles between flare-ups and symptom-free remissions, with durations varying.
Flare-up symptoms include:
- Dry and scaly skin.
- Itching (or pruritus).
- Skin lesions: raised, red, irritated patches giving the skin a rough, swollen appearance. Blisters on these patches break, leading to oozing and crusting.
Over time, affected skin can become discolored, thicker, and drier (lichenification).
The symptoms of atopic eczema
Dry and scaly skin
Itching
Skin lesions
Atopic dermatitis affected areas¹ ³
The location and appearance of atopic eczema lesions vary by age:
- In infants under two years, lesions are often red, weeping, mainly on the face, arms, and cheeks.
- From 2 to 12 years, lesions are drier, with crusts and scales due to scratching, typically on the elbow and knee folds.
- In adolescents and adults, thicker lesions affect elbow and knee folds, as well as the face, eyelids, neck, wrists, feet, and backs of hands.

Differentiating eczema from other skin conditions
Several skin conditions may mimic eczema symptoms (such as patches, redness, itching, scales, or flare-ups), making diagnosis challenging.

Psoriasis
This non-contagious inflammatory skin disease features thicker, well-defined red patches with significant scales, often on the elbows, the knees, and the scalp.
Seborrheic dermatitis
A common inflammatory skin condition affecting sebum-rich areas like the scalp and face, characterized by pink or salmon-colored patches with thick, greasy scales.


Scabies
Unlike eczema, scabies is an infectious disease caused by a parasite, leading to red bumps and intense itching. Doctors may look for burrows, which are traces of the parasite in the skin.
Urticaria
Urticaria lesions are superficial, swollen, rounded, resembling nettle rashes.


Fungal infections
Candidiasis and dermatophyte infections often develop in warm, moist body areas, like major folds (groin) and minor folds (in between toes). Outside these areas, dermatophytes sometimes present a characteristic "ring" appearance.
Understanding the causes and triggers of atopic eczema
Eczema: a multifactorial disease¹ ³ ⁴
Eczema's exact causes are not fully understood, but it results from a mix of genetic, immune, and environmental factors:
Genetic component: people with eczema often carry a mutation of the filaggrin gene, affecting the skin's outer layer formation. Consequently, their skin is permeable and less effective at retaining moisture and protecting against external substances such as irritants, allergens, and microorganisms. Furthermore, their epidermis contains fewer beta-defensins proteins, which are important for fighting bacteria, viruses, and fungi.
Reactive immune system: individuals with atopic dermatitis have an overreactive immune system, producing excessive allergic-type (IgE) antibodies in response to environmental allergens like dust mites, animal hair, or pollen.
Environmental influences: various environmental factors can trigger eczema flare-ups, such as soap, rough fabrics, certain foods, weather conditions, sweat, cigarette smoke, pollution, bacterial and viral infections.
Atopic eczema triggers¹ ³ ⁴
Atopic eczema triggers are individual and vary from person to person, commonly including temperature changes, hot showers, hygiene products, perfumes, irritating textiles, and stress.
The triggers of atopic eczema
Temperatures variations
Fragrance
Stress
Is atopic eczema dangerous ?
A "benign" disease¹ ³
Eczema isn't life-threatening but can be very uncomfortable, significantly affect health and well-being, or lead to other complications.
Complications of atopic eczema¹ ³
1. Lichenification: chronic eczema causes a change in skin texture, becoming rough and thick, known as "lichenification."
2. Skin Infections: damaged skin, especially from scratching, becomes vulnerable to bacterial, viral, and fungal infections.
3. Sleep disorders: severe itching can disrupt sleep, affecting overall health and well-being.
4. Psychological issues: Managing a chronic condition, itching, and discomfort can lead to anxiety and depressive disorders.
Complications of atopic eczema
Lichenification
Skin infections
Sleep disorders
Psychological disorders
Effective eczema treatments
The treatment of atopic eczema primarily focuses on symptom relief during acute episodes and proactive measures to prevent future flare-ups.
Treating eczema flare-ups³ ⁶ ⁷
Doctors typically prescribe topical corticosteroids, available as creams or ointments, to directly alleviate inflammation and itching during flare-ups.
Preventing disease flare-ups³ ⁶ ⁷
A key aspect of eczema management is the daily hydration of the skin, crucial for maintaining long-term disease control. Emollient are instrumental in reinforcing the skin's barrier function, ensuring it remains healthy and flexible. They effectively combat dryness, alleviate itching, and minimize flaking. For optimal results, apply these emollients across the entire body once or twice daily, ideally following a brief shower and gentle pat drying. Opt for fragrance-free emollients that feature a straightforward formula with minimal ingredients for the best care.
FAQ
Atopic eczema (or dermatitis) is a inflammatory skin disease (hence its other name of dermatitis), which develops in chronic flare-ups, i.e. alternating between phases of calm and symptomatic phases. Atopic eczema has 3 main characteristics: itching, inflammatory skin lesions and dry skin (or xerosis).
Skin infections may occur as a result of skin irritation, particularly in eczema lesions. Consult a doctor if you have any concerns.
It is indeed important to discuss the necessary precautions with teachers. You can provide them with information on atopic dermatitis through documents available on certain information sites such as the Eczema Foundation website https://www.pierrefabreeczemafoundation.org/etre-accompagne/supports-et-outils, discuss the necessary precautions and ensure that teachers are informed of any medication your child is currently taking.
References:
1. L’Assurance Maladie. Eczéma ou dermatite atopique : causes, symptômes et évolution. Ameli.fr. Septembre 2023. [Disponible sur :] https://www.ameli.fr/assure/sante/themes/eczema-atopique/reconnaitre-eczema-atopique
2. American Academy of Dermatology. Eczema: types and treatments. AAD. 2023. [Disponible sur :] https://www.aad.org/public/diseases/eczema/types
3. Nemeth V, Evans J. Eczema. National Library of Medicine. Août 2022. [Disponible sur :] https://www.ncbi.nlm.nih.gov/books/NBK538209/
4. INSERM. Dermatite atopique (eczéma atopique). Une maladie chronique inflammatoire de la peau fréquente. INSERM.fr. Juillet 2017. [Disponible sur :] https://www.inserm.fr/dossier/dermatite-atopique-eczema-atopique/
5. Barrett M, Luu M. Differential Diagnosis of Atopic Dermatitis. Immunol Allergy Clin North Am. Février 2017.
6. L’Assurance Maladie. La consultation et le traitement en cas d'eczéma ou dermatite atopique. Ameli.fr. Septembre 2023. [Disponible sur :] https://www.ameli.fr/assure/sante/themes/eczema-atopique/consultation-traitement
7. Wollenberg A and al. European guideline (EuroGuiDerm) on atopic eczema - part II: non-systemic treatments and treatment recommendations for special AE patient populations. J Eur Acad Dermatol Venereol. 2022 Nov;36(11):1904-1926.
- Discover The Different Types of Eczema: How to Recognise Them?
The Different Types of Eczema: How to Recognise Them?
- Discover Causes of Eczema: Why Does It Occur and How Can You Prevent It?
Causes of Eczema: Why Does It Occur and How Can You Prevent It?
- Discover Eczema Symptoms: Identification and Understanding
Eczema Symptoms: Identification and Understanding

















